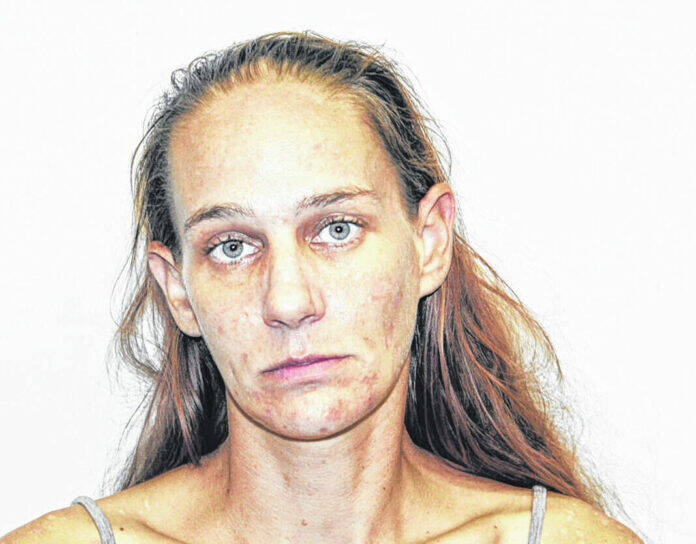
Ashlee R. Fletcher
By Meladi Brewer
DailyAdvocate.com
GREENVILLE — Medical professionals testified on Wednesday to the dangers a small illness can have on someone with diabetes. Judge Travis L. Fliehman presided.
“Anytime a child comes in with DKA (diabetic ketoacidosis), many times they come in because they may have a little illness,” the diabetes educator said. “For a diabetic, anytime that the child is ill it is really important to closely monitor the ketones and blood sugar every three to four hours.”
She said it is because any simple illness can cause the child to go into DKA which is a medical emergency. The educator advised that the day prior to the child presenting with DKA, his glucose readings were high, meaning they were over 600. Detective Morrisa Reed testified that during her investigation, Fletcher told her she had been monitoring her son since he came home.
In a recorded interview with Fletcher, viewers could hear Fletcher advise Detective Reed that she knew to give her son insulin every two hours and gave times when she administered the doses. She could be heard saying she got her son home around 7 p.m. when she gave him nausea medication. She advised she gave him his daily 9 p.m. shot before administering another at 11 p.m. and 1 a.m. She also gave him more nausea medication around midnight.
“I know I got him insulin, and I know I gave him his 9 o’clock shot,” Fletcher said. “I know I checked it at one point because it was reading high, and I gave him insulin every two hours. Then the blood checker read 378, but I might be wrong”
Data pulled from the Dexcom showed elevated levels in the victim’s blood.
Fletcher also advised the detective that her son refused to pee on the stick, as she was not in the bathroom with him.
It had been testified by previous medical professionals that the level of ketone in the system determines how much insulin is needed to be administered, and Fletcher was given a chart for reference. She told the detective it is better to give less insulin than too much.
“I assumed he had ketones in there, and I would give him a little bit more- like one unit more because I didn’t want him to not have it and give way too much to drop his sugar,” Fletcher said. “It is better to have less, but I was worried if he didn’t have ketones because I didn’t know.”
She said giving him too much insulin would have “bottomed him out especially without him eating anything.” She said she can give him insulin every two hours, but at that time she couldn’t give him food or water because it would come back up. She said her son had thrown up “about 20 minutes” before she went to bed. Fletcher went to bed around 3 a.m. and not get up until 1 p.m. the next day.
Detective Reed also showed text messages where Fletcher had sent a picture of her son, dead on the couch to two different people. It was testified by the neighbors, who told her to call 911, EMS, and firefighters that no one witnessed her take a picture of her son after their arrival. They did, however, testify to her talking and arguing on the phone while they tried to resuscitate her son. One fireman testified in his years of experience it is unusual for someone to be on their phone outside instead of glued to the patent.
Detective Reed said after all the interviews with dad and Fletcher, she knows, according to Fletcher and doctors, that the child could have insulin every two hours, Fletcher showed her a timeline that she administered five shots the night he came home.
“He hadn’t had dinner, he couldn’t keep down water, she said she would not be able to hear him if he got up to go to the bathroom,” Detective Reed said. “She tells me of a shot she gave him at 1 a.m. in the morning and then she doesn’t describe anymore shots.”
Detective Reed said the victim “didn’t have breakfast or a snack, he didn’t have lunch, didn’t have any insulin,” and then Fletcher found him unresponsive at 1:30 p.m.
Fletcher stated in the interview why she had left the hospital that evening saying it wasn’t just because her ride had been leaving. “I knew. It’s why I left him the night before. I have never left him at the hospital,” Fletcher said. “I left because I already knew we’re not taking him home.”
Fletcher could be heard telling Reed she left to give her son’s dad time to know that their son was not going to wake up. She said she needed his dad to agree to take their son off life support because she was not going to do it without him agreeing, and needed him to make the decision.
The victim’s doctor at Dayton Childrens advised the victim had been in shock upon coming into the ER and ICU that day. He advised shock can be caused by low blood pressure, severe dehydration, and more that causes the body to not circulate oxygen.
The doctor said with diabetes you are at very high risk of becoming dehydrated because you have sugars that can build up in you blood stream and your body pushes fluids out to try and break the sugar down. He said being dehydrated can lead to shock.
“It appears to have been days of dehydration in my estimation,” the doctor said. “It would be hard to get that dehydrated in just a couple of hours.”
Upon arrival to the ICU, the doctor knew the victim was in a rough state, as in his 17 to 20 years, he has taken care of only a half a dozen kids who have been as sick as the victim.
Fletcher’s female neighbor testified to having witnessed Fletcher the night before and day of the victim passing. She said she saw Fletcher helping the victim inside because he was too weak to walk on his own.
“I was concerned because she was practically carrying (him) into the house like somebody who is drunk and can’t walk,” the neighbor said.
This story correlated with one of the two stories she had told the father. A male firefighter advised Fletcher had told him her son had been a diabetic for years and had been sick for a couple of days. When he inquired about when the patient had last been talked to, he said he got three conflicting times.
The neighbor had asked the night before why Fletcher had not taken her son to the hospital, and she said her son didn’t want to go.
“I was kind of confused by that statement because he is a child,” the neighbor said.
Fletcher had also told the neighbor he had been sick at his dad’s, and dad had brought him to her work. Dad carried him to her car, and she brought him home instead of to the hospital. She was told by Fletcher the dad was not allowed to take the victim to the hospital.
“She told me dad wasn’t allowed to,” the neighbor said. “That he didn’t have rights to him.”
The victim’s school nurse was the last state witness of the day. She testified the male would see her three to four times a school day for monitoring and treatment for years, as he had been diagnosed as a second grader. She said she treated him per doctor’s orders for the medical diagnosis.
The last day she saw the victim was May 5, 2022. He came down saying his mom told him to take a nap for strength for the state testing that had been done. When she asked what that meant, she was heartbroken by the answer. “He said had been vomiting for a week and a half, he didn’t feel good, and he wanted to go to the hospital,” the nurse said.
His sugar reading was off the meter and very high. His ketones were “very, very high” and the nurse gave him insulin, gave him water, and got him breakfast. When she called mom and told him he needed to go to the hospital, Fletcher told her she couldn’t leave work and to bring him to his step grandma’s house across the street.
“She was at work. She couldn’t leave work to come get him, and I told her he doesn’t feel well and wants to go to the hospital. I want him to go to the hospital,” the nurse said.
Defense Attorney David Rohrer questioned the nurse about calling CPS if she was a mandatory reporter with all the data she had plus concerns that day, and she said she had called CPS in November of 2021, and she did not call that day because the mother said she would call the doctor. The nurse said she did call the doctor to give them a heads up on the situation and to say mom was to call the doctor.
State Prosecutor Deborah Quigley objected to Rohrer’s constant CPS question and stated that CPS was not on trial for what they did, but rather they were there to determine if the defendant did what she was supposed to do regardless of what everyone else may have done.
From there she recross examined the witness about calling CPS, and the nurse said multiple staff members had called over time while the victim had been in their care.
To contact Daily Advocate Reporter Meladi Brewer, email [email protected].