
GREENVILLE – Health care professionals today will argue they are working in the fastest-changing profession in the country. And, according to national and state hospital associations, the industry is dealing with a number of game changers that are shaping its landscape.
Representatives from the American Hospital Association (AHA) and Ohio Hospital Association (OHA) are speaking to this fact and traveling to hospitals sharing information about national and state health care and helping local communities facilitate discussions on health care trends, challenges and opportunities; health care transformation and what the future holds.
Recently, Wayne HealthCare was the first community hospital in Ohio to host a community strategic planning meeting in partnership with the American Hospital Association, the Ohio Hospital Association, Wayne HealthCare Board and Foundation Board members, Wayne HealthCare leadership and management and Coalition for a Healthy Darke County board members. The meeting had about 60 attendees.
“I would just like to thank AHA and OHA leadership for choosing Wayne HealthCare as the first hospital in Ohio to make their presentation,” said Wayne HealthCare President/CEO Wayne Deschambeau. “They have solicited our input to the healthcare community’s attitude and expectations to the evolving health delivery and wellness system in Ohio and throughout the USA.”
In an introduction, Deschambeau talked about the importance of joint ventures offering an example of the hospital’s most significant one – the Wayne Cancer Center, an affiliation between Wayne HealthCare, Good Samaritan Hospital, Miami Valley Hospital and Dayton Physicians, LLC.
“It’s been a very successful program,” said Deschambeau. “We invested $400,000 in the project about four years ago which has completely paid itself off in return. We [the hospital] have a 5-percent ownership of radiation oncology services which is a group of six cancer centers throughout the Miami Valley.”
Deschambeau spoke of other partnerships with Reid Health in Indiana for Continuing Medical Education classes and becoming a recent member of the Ohio State Health Network, with Ohio State University Medical Center.
Competition was another topic in the forefront.
“I’ve been here about 10 years now and when I came here it would be fairly safe to say that Wayne Hospital really didn’t have any competition…That whole environment has changed a little bit more dramatically,” he said.
Deschambeau said he was seeing more of what he called, “doc in the boxes,” or walk-in clinics, for people seeking additional care. Another concern was chain retailers or grocery stores beginning to offer nurse practioner clinics.
“The entire environment continues to change and one of the things I think that we’ve been very pleased with here [at Wayne HealthCare] is all of these potential competitors have really kind of opened their doors to us, to talk about things that we can do,” he said.
Wayne HealthCare Survey
Prior to the meeting, attendees were asked to participate in a 10-question, confidential, survey that posed questions about local healthcare. It was used to prompt group discussion at the end of the meeting.
The results of the survey are as follows:
Results showed that participants thought chronic illness and mental health issues (including drug abuse) were top health care challenges facing the community, with affordability and access to care trailing behind.
Participants felt better coordination of care was the largest obstacle facing the community over the next five years with the cost or price of care coming in as a second choice and access to other health care services in the community and need for preventative care as their last choices.
More primary care physicians/providers in the future to improve the community’s health topped the list for participants, with urgent care services, social services, home health and other services trailing.
Participants agreed that in the next five years, compared to today, most patients in the community will have electronic health interactions (scheduling appointments, getting test results, medical records, etc.).
Survey-takers also agreed that hospitals should partner with business and others in the community to impact health challenges.
Participants were asked if over the next five years they foresaw any changes in the current hospital as it relates to possible mergers, acquisitions or affiliations with other health care organizations. Many participants expressed the need to explore such options in the form of collaboration, consolidation or affiliation; some said they were aware of current partnerships and it was even expressed as a necessity for the hospital to do so for survival.
Survey-takers felt the hospital would have fewer in-patient beds in the next five years.
Compared to today, participants felt, in the next five years, health care will be more integrated and providers will be paid based on a fixed price for all care that is delivered versus reimbursed on each service provided.
Participants also felt that compared with today, hospital payments in the future will be based on the value of the services provided rather than the volume or number of services.
An opportunity was given for participants to ask their own question to be used in the discussion portion of the meeting regarding health care services in the community. Questions ranged from additional health care services, the need for more primary care physicians to customer service which the hospital offers.
Community Discussion
Towards the end of the meeting, attendees were broken into groups to discuss barriers to accessing care in the community. A recap of items discussed were provided to the hospital for further examination.
Patient denial of health issues; decline of services; poverty; mental status; multi-generational substance abuse; access of information; communication through school, work, neighbors, friends, billboards, newspapers, radio, TV; family support systems; and challenges of compliance were some of the topics briefly discussed.
National health care landscape
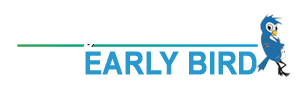
Kim Byas, Sr., PhD, MPH, FACHE of the American Hospital Association spoke about the national health care landscape in his presentation, Redefining the “H”: The Road to Health Care Transformation.
On the national level, Byas proposed looking at:
- The political landscape (diversity in the U.S. electorate, or lack thereof);
- U.S. population characteristics (baby boomers’ life expectancy with chronic conditions, palliative care, behavior genetics and social factors and mental illness);
- National health insurance trends (impact of the Affordable Care Act, employee health plan changes, exchange carrier networks);
- Physicians (due to payment shifts by 2019 from volume to value, more are likely to retire earlier, move into mega groups or become employed by hospitals/health systems or insurers);
- Healthcare workforce (increased hospital CEO turnover, concerns about finding qualified people, private sector health care employment falling);
- Information and technology (major platform or strategy for advancing in payment and delivery, care coordination of patients, satellite, drones, smart phones, etc, will force adaption and innovation); and
- Patient safety and quality (Medicare readmission rates have declined, palliative and end of life care needs addressed).
Health system transformation is a big topic of discussion as it will change the way in which hospitals will operate in the future.
According to Byas, 86 percent of health care CEOs believe technological advances will transform their businesses in the next five years. Demographics will also force transformation in customer growth and retention.
Byas said that unsustainable health care costs and an inordinate share of Gross Domestic Product are forcing the U.S. health care system to transform from hospital-centric sick care to a super outpatient model that will emphasize community-based care.
He also said hospitals are increasing scale through horizontal and vertical integration and moving toward better collaboration, prioritization of programs, increasing purchasing power, consolidating services and cutting costs.
Additionally, practitioners, payers, patients, and policymakers are demanding value, best outcomes, and transparency.
Byas presents that in the next five years, the nation will see more hospitals in systems; more physician affiliation with hospitals; more providers owning health plans; more value-based payments and more fixed/capitated payment.
With a prediction of more hospitals in the future, the AHA Committee on Research in its January 2014 report identified five potential paths for hospitals of the future:
- Partner: With a care delivery system or health plan
- Experiment: With new payment and care delivery models
- Integrate: By developing a health insurance function or services across the continuum of care
- Redefine: To a different care delivery system
- Specialize: To become a high-performing and essential provider
Ohio health care landscape
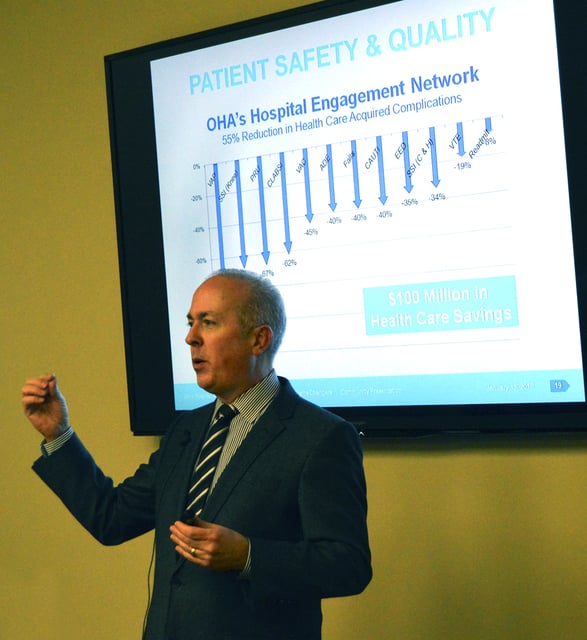
Mike Abrams of the OHA talked to the group about game changers in the healthcare landscape throughout the state.
“Whether you’re a CPA or whatever industry you might be in, you’re all undergoing change,” said Abrams. “But, I would dare anybody to explain that the pace of change in their industry is faster than the pace of change in health care. It’s enormously fast in health care.”
One game changer Abrams pointed out was technology.
“For many years when technology would meet your industry, you would become more efficient…and the cost of your product or service would decrease and that’s good,” he said. “The opposite has been true in health care…when technology is introduced to health care, the costs go up, now there’s value added, you’re getting something for that, but it is going up.”
Abrams said in the past, as technology advanced in health care, costs have risen. Today, he said, new technology is helping to bring costs down, citing an example of DeepMind technology (artificial solve intelligence acquired by Google in 2014) being used to read mammograms at MD Anderson Cancer Centers in Texas.
“These kinds of game changers are, I think, the result of a very impatient economy that has been dissatisfied with how the health care system has been, frankly, unresponsive to some of the things they believe that we should be doing more efficiently,” he said.
Another game changer, a positive one, Abrams said, was the state’s Medicaid expansion.
More than 500,000 Ohioans are now covered under expanded Medicaid criteria, said Abrams. And, 200,000 people purchased coverage on the health care exchange.
“Now more than half a million of our citizens are enjoying health care coverage in a more responsible way,” he said. “Before, they were the chronically-ill patients, who had limited access and very sub-optimal access to the health care system, so instead of managing their chronic condition over a period of time, many times they would wait until a catastrophic manifestation that showed the ER a very interesting, complicated patient. Now they have the opportunity to change that.”
The downside is that hospitals are facing population health challenges throughout the state. Obesity, smoking and low birth weight in infants are at the top. Ohio ranks no. 39 in overall health in the U.S.
“We were the 4oth healthiest state in the country a couple of years ago. The new rankings just came out… and showed that we are trending in the right direction, however, we are no. 39,” said Abrams. “We were recently 50th in the nation for black infant mortality and 47th for overall infant mortality. Those numbers are actually getting better from overall infant mortality, but worse from the black infant mortality standpoint.”
Abrams said that as long as the data was problematic there would never be an inexpensive health care system in the state of Ohio.